One of the questions I’m asked most often—especially by hospital systems—is where Occupational Medicine should report. HR? Legal? Ambulatory? Employee Health? Risk?
After working with hundreds of NAOHP member programs over the years, I can tell you this: there is no single universal structure, because every organization brings its own priorities, history, and culture.
Some are primarily focused on internal employee health and compliance.
Some operate robust external employer-service lines.
Some do both.
Some are rebuilding.
Some are scaling rapidly.
And we support all of them.
But across all these variations, one theme is very clear.
Programs thrive when Occupational Medicine is treated as a clinical, worker-focused service line—not a legal function.
Among our NAOHP membership, I’ve seen programs reporting into almost every imaginable place:
- Ambulatory services
- Urgent care leadership
- Employee Health
- Risk Management
- HR/People Services
- Population Health
- A few placed under Legal
Each structure reflects what the organization values most—internal safety, regulatory compliance, growth, employer relations, or operational consistency.
Yet the programs with the strongest outcomes, the highest employer satisfaction, and the best worker experience (internal and external) almost always share the same foundation:
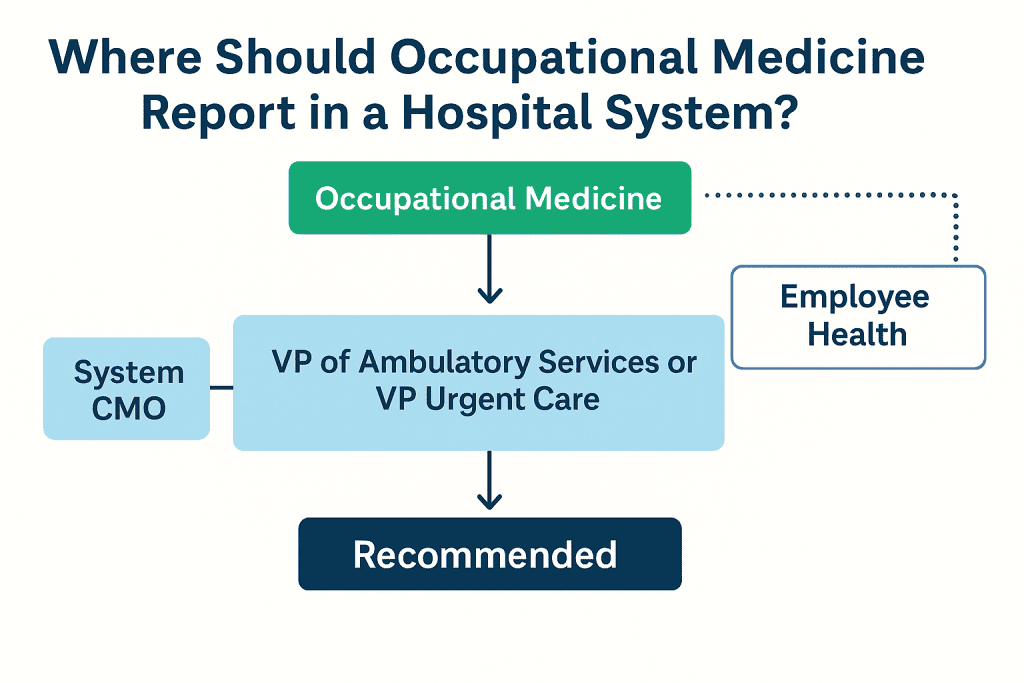
Occupational Medicine reports through clinical operations—usually Ambulatory or Urgent Care—with medical oversight through the system CMO and a collaborative, not adversarial, relationship with HR, Employee Health, and Risk.
Why legal reporting rarely works
A handful of systems have placed OccMed directly under Legal or Compliance. I understand how that happens—especially after an OSHA citation, workers’ comp event, or internal audit.
But legal-based reporting almost always becomes adversarial at its core:
- Every decision is filtered through liability
- Every discussion becomes about minimizing exposure
- Clinical judgement takes a back seat
- Employer relations suffer
- Worker trust erodes
This structure protects the institution, but not the worker—and in Occupational Medicine, those two things are inseparable. If you undermine the worker relationship, you weaken both compliance and outcomes.
And regardless of whether you’re serving your own workforce or external employers, the principle is the same:
A worker-first approach is the only path that leads to strong clinical outcomes, sustained employer partnerships, and a positive safety culture.
Legal plays an important consultative role—but it should never be the primary supervisory layer for this service line.
What actually works for hospital systems
Across the wide variety of programs in our NAOHP community—from small rural hospitals to multi-state integrated systems—the structure that consistently supports strong performance is:
1. Occupational Medicine reports to Ambulatory Services or Urgent Care
- Clear operational support
- Strong scheduling and workflow infrastructure
- Alignment with other clinical access points
- Ability to scale and grow employer services
- Visibility as a revenue-generating service line
2. Medical oversight sits with the system CMO or Ambulatory CMO
- Ensures clinical rigor
- Maintains regulatory alignment
- Creates consistency across providers and sites
3. Employee Health stays within HR but partners closely with OccMed
This lets both internal and external priorities thrive without conflict.
4. Risk Management and Legal act as advisory partners
Not supervisors.
Why this matters for both internal workforce and employer clients
Whether you’re managing your own employees’ injuries or supporting regional employers with pre-employment, surveillance, and RTW services, the goal is the same:
Protect the worker.
Support safe work.
Keep people healthy and productive.
This is the philosophy shared across NAOHP—regardless of how big the program is or which department it sits under. It’s also the philosophy that has helped our members grow and elevate the value of Occupational Medicine inside their systems.
A clinical, worker-first alignment helps:
- Strengthen OSHA and workers’ comp performance
- Improve recordability accuracy
- Build trust with employees
- Build long-term employer partnerships
- Expand the service line responsibly
- Reduce friction between departments
- Make the program visible as both a safety asset and a business asset
A final thought
Every system’s structure is a little different, and NAOHP supports that diversity. But if you’re evaluating your own alignment—or you’re considering a restructure—the guiding principle I come back to is simple:
Occupational Medicine succeeds when it is positioned as a clinical service line with a collaborative, worker-first mission—not a defensive, adversarial one.
That’s true for internal employee health, and it’s true for external employer services.
👥 Member only resources:
How Hospital Systems Structure Occupational Medicine Infographic, Practice brief, slide deck, Employer positioning statement
📚 References & Supporting Evidence
NIOSH Total Worker Health®
- NIOSH. Total Worker Health® Program: Fundamentals of Integrated Approaches. CDC; 2018.
- NIOSH. Fundamentals of Total Worker Health Approaches: Essential Elements. DHHS (NIOSH) Publication No. 2016-117.
ACOEM Guidance
- ACOEM. The Role of the Occupational Medicine Physician. JOEM. 2019.
- ACOEM. Occupational Health Services in Health Systems: Principles for High-Value Care. ACOEM Guidance, 2020.
- ACOEM. Code of Ethical Conduct. 2020.
American Hospital Association (AHA)
- American Hospital Association. 2023 Health Care Workforce Scan.
- American Hospital Association. Trends in Ambulatory Care and Employer Partnerships. 2022.
Joint Commission Standards
- Joint Commission. Human Resources (HR), Leadership (LD), and Infection Control (IC) Standards. 2021–2024 editions.
AAOHN / ANA
- AAOHN. Competencies and Guidelines for Occupational and Environmental Health Nursing. 2018.
- AAOHN & American Nurses Association. Scope and Standards of Occupational Health Nursing Practice. 2016.
OSHA Recordkeeping & Regulatory Guidance
- OSHA. 29 CFR 1904: Recordkeeping Standard.
- OSHA Interpretation Letters (multiple) emphasizing determinations by “licensed healthcare professionals.”
Workers’ Compensation Research Institute (WCRI)
- WCRI. The Early Impact of Clinical Models on Workers’ Compensation Outcomes. 2020.
- WCRI. Return-to-Work Practices in Large Systems. 2019.
Major Health System Models (Published & Public Summaries)
- Mayo Clinic. Occupational Health Services Overview. Mayo Clinic Proceedings. 2020.
- HCA Healthcare. Occupational Health Service Line Overview. Summaries from Ambulatory Division reports (2021–2023).
- Kaiser Permanente, Sutter Health, Intermountain Health — published service line briefs on employer programs.
Urgent Care Association (UCA)
- UCA. 2022–2024 Benchmarking Reports: Employer Services & Occupational Medicine Trends.
Institute for Work & Health (IWH)
- Institute for Work & Health. Organizational Policies That Improve Return-to-Work Outcomes. 2017–2021.
RAND Corporation
- RAND. Employer Health Programs: Structural Determinants of Success. 2020.
Harvard T.H. Chan School of Public Health
- Harvard T.H. Chan School of Public Health. Leading in Total Worker Health. 2021.
Safety & Culture (CDC / NIOSH)
- CDC/NIOSH. Safety Climate and Worker Health. 2015–2020.
- CDC. Impact of Organizational Culture on Injury Outcomes. 2019.
Legal Oversight – Reasons Against Direct Reporting
- American Bar Association (ABA). Legal Oversight in Clinical Environments: Risks of Role Conflict. 2017.